I have the good fortune to take care of a many number of patients with a Chiari malformation, so I thought I’d use this opportunity to talk a little bit about it.
There are multiple types of Chiari malformations, one, two, three, Chiari four. Three and four are pretty rare and I’m not going to discuss them today, nor Chiari two which is associated with Myelomeningocele or what people commonly call, Spinal Bifida–very, very different entity even though it shares the same name. So, I’m going to focus on Chiari one malformation, which is the patients that I care for and get asked quite a bit about this.
Many people, maybe, suffering from a headache or some other problem and they’ll go get an Mri of their brain and the radiologist will read the film and say that there’s a Chiari one (Chiari I) malformation and seek neurology, a neurosurgical consultation.
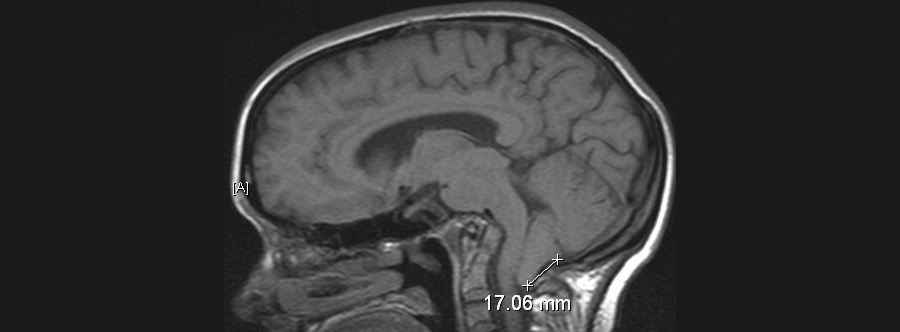
People come in all scared and they have this problem and want to know what they need to do. So the radiologist will read a Chiari malformation when the back part of the brain, an area called the tonsils of the Cerebellum, which is way back here under those thick muscles in the skull. When those droop down through the hole at the base of the skull, if they droop down more than a few millimeters, they’ll say there’s a Chiari malformation. That’s technically what it is based upon the MR–the imaging data. However, the vast majority of people who have droopy tonsils that droop down a little bit, they don’t need anything done for this “Chiari malformation” and it’s just a finding–maybe like having a bigger nose than somebody else or a droopier ear lobe or something like that. It really, really is of no consequence.
So the question is, is how do you figure out which patients that Chiari is a problem and what you should do about it and which patients you shouldn’t–you should just leave them be.
This is where it gets a little complicated, but our brains float in some fluid and every time our heart beats, every time we take a deep breath, our brains pulsate and anybody who’s looked closely at a newborn (there’s a little soft spot at the top of the head), you can actually watch the fluid pulsating at the top of the head. Well, as an adult, are soft spot is gone. Our skull is solid, so when our brain pulsates, no our eyes don’t pop out with every pulsation. What happens is the fluid that’s around the brain has to rush out of the skull and it rushes down through the hole at the base of the skull, this frame and magnum. Then when the brain shrinks, that fluid has to rush back up again. With every breath and with every heartbeat, the brain pulsates just like the heart does–that fluid has to flow in and out, so that the brain can expand and then shrink, expand and then shrink. Well, if those tonsils, that back part of the brain, goes down that hole and it’s too snug, then the fluid can’t flow back and forth the way it should. If the fluid can’t flow back and forth the way it should, then it can cause lots of trouble–commonly things like headache and pain at the back of the neck or problems when you cough or grunt, you know, like having a bowel movement. These are situations where that fluid flow problem gets accentuated and it becomes even more problematic and that’s where potentially a neurosurgeon needs to help fix that fluid flow problem.
Those are the patients with Chiari that need something done. Now, if I get a patient in my clinic and they have intermittent headaches and they have this Chiari, even if I think they might be having some fluid flow problems, sometimes caution (or often times caution) is the best way to go. Don’t rush off to surgery. In a day of clinic, it’s not uncommon for me to see one or two or even three patients who were referred to me for the Chiari symptoms and for this descent of the tonsils, and yet, I operate on very few of these patients–probably less than 10 percent, even maybe as low as five percent.
What you have to understand is two things: One, this is typically in younger people, it’s typically in late teens through early thirties that we see people coming in and I want you to think about how common headache is in this group. Lots of use of coffees and teas and other stimulants, or these energy drinks, lots of sleep deprivation–whether from school needs or partying–lots of stressors at early points in the life, new parents, new jobs, moving, lots of things go on in these early years. Getting headaches is a pretty common thing. Nowadays, so many people have access to getting MRI’s. You take a common problem, headaches, you get a lot of MRI’s and next thing you know, you’re going to find a significant number of people have this modest amount of descent of the tonsils. The key here is most of these people don’t need surgery. You really don’t want to go operating on somebody because they have headaches and do a surgery that potentially could even cause headaches, so caution is always the best way.
If the problem is very dramatic and the fluid flow problem is really a big issue, usually what I will do is get a special type of MRI where I can actually look at the fluid flow on the MRI. It’s a movie MRI instead of a static MRI, and I can make sure that I can see that the fluid’s blocked or that it actually is flowing. If the fluid’s flowing, then that really proves that the fluid flow is not the issue and so trying to fix the Chiari isn’t indicated.
If that movie MRI, or what we call a Cine–MRI, shows that the fluid is obstructed and the symptoms are really disabling, and you’re confident and the patient’s confident that these things are related than as a surgeon what I can do is I can go into the back of the head here and I can open up some of the skull, open up some of the covering that’s over this area, and make that hole at the base of the skull bigger. That allows the tonsils to still stay where they are, but this allows the fluid now to rush around it. This can be a very, very rewarding operation for patients who are suffering from these problems because it can really help, tremendously, alleviate these symptoms.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing relating symptoms, please visit your doctor or call 9-1-1 in an emergency.
Read More from Dr. Charles Rosen
Multiple Aneurysms: Emilia Clarke
I'm getting a lot of questions these days about aneurysms and Emilia Clarke, the game of Thrones star, and the unusual aspect of her history is to having multiple aneurysms that needed care, so I wanted to talk a little bit about how often we see that. The...
read moreBrain Eating Amoebas
Last year I got asked a lot about the terrible tragedy related to the brain eating Amoeba or brain eating bug as it's called in the press. First off, these are relatively uncommon. They are horrific when they occur, but they're not common. What it is, is...
read moreHeat Stroke
With the temperature increasing, as a motorcyclist, I'm very aware of the issues of heat exhaustion and heat stroke, and these are very dangerous issues. Our bodies need to stay at a standard temperature (98.6 degrees Fahrenheit, 37 degrees Celsius), and...
read more